
Acute coronary syndrome (ACS) is a term encompassing conditions like unstable angina, non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI), caused by reduced coronary blood flow leading to myocardial ischemia or infarction. It is a medical emergency requiring prompt diagnosis and treatment to improve outcomes and reduce mortality.
1.1 Definition and Overview
Acute coronary syndrome (ACS) is a spectrum of clinical conditions caused by reduced blood flow to the heart muscle, leading to myocardial ischemia or infarction. It encompasses unstable angina, non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI). ACS is characterized by chest pain or discomfort, often accompanied by electrocardiographic changes or elevated cardiac biomarkers. It represents a medical emergency requiring immediate evaluation and treatment to restore coronary blood flow and prevent further cardiac damage. Prompt intervention is critical to improve outcomes and reduce mortality.
1.2 Pathophysiology of ACS
Acute coronary syndrome (ACS) primarily results from atherosclerotic plaque disruption, leading to coronary artery thrombosis. Vulnerable plaques, characterized by a thin fibrous cap, large lipid core, and high macrophage density, are prone to rupture. This triggers an inflammatory response, platelet activation, and fibrin clot formation, causing partial or complete artery occlusion. Reduced blood flow leads to myocardial ischemia or necrosis, depending on the severity and location of the blockage. This pathophysiological process underpins the clinical manifestations of ACS, necessitating urgent intervention to restore coronary perfusion.
1.3 Classification of ACS
Acute coronary syndrome (ACS) is classified based on clinical presentation and diagnostic criteria into three main types: unstable angina, non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI). Unstable angina is characterized by chest pain at rest or worsening angina without evidence of myocardial necrosis. NSTEMI involves myocardial damage with elevated biomarkers but no ST-segment elevation on ECG. STEMI is identified by ST-segment elevation on ECG and significant myocardial necrosis, requiring urgent reperfusion therapy. This classification guides treatment and prognosis.
1.4 Clinical Importance and Epidemiology
Acute coronary syndrome (ACS) is a major cause of morbidity and mortality worldwide, accounting for a significant proportion of hospital admissions. It is a leading cause of death globally, particularly in low- and middle-income countries. The global burden of ACS is increasing due to rising rates of cardiovascular risk factors such as hypertension, diabetes, and obesity. Timely recognition and management are critical, as ACS is associated with high healthcare costs and long-term societal impact. Prevention strategies remain essential to reduce its global burden and improve outcomes.

Risk Factors and Etiology
Acute coronary syndrome (ACS) is linked to modifiable and non-modifiable risk factors, including hypertension, diabetes, hyperlipidemia, and smoking. Plaque instability and rupture, often triggered by inflammation, underpin its etiology, leading to coronary artery obstruction and ischemia. Genetic predisposition and advancing age further contribute to its development; Understanding these factors is crucial for prevention and targeted interventions to reduce the global burden of ACS. Early identification and management of risks remain key to improving outcomes.
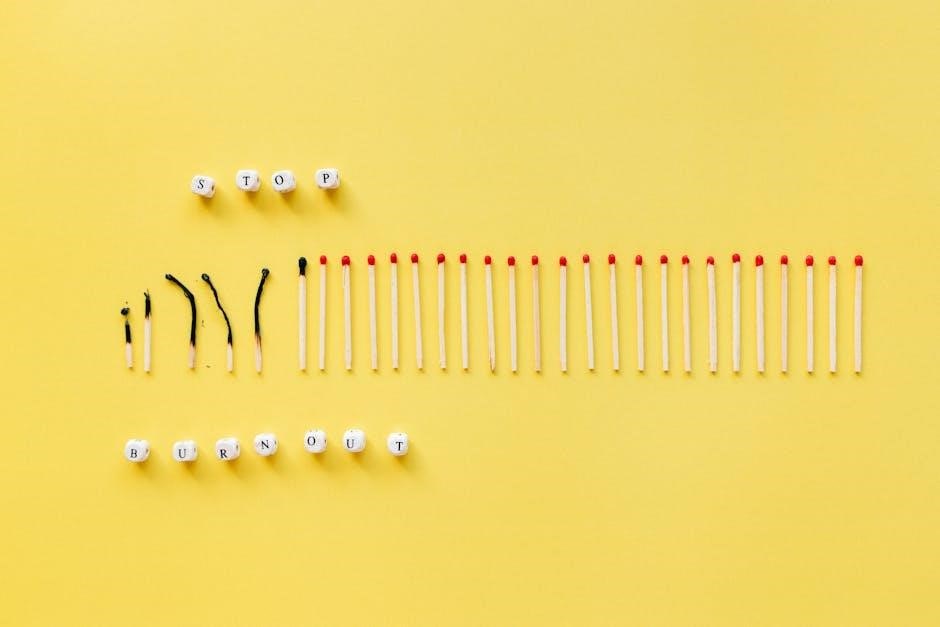
2.1 Modifiable Risk Factors
Modifiable risk factors for acute coronary syndrome (ACS) include hypertension, hyperlipidemia, diabetes mellitus, smoking, and obesity. These factors contribute to the development of atherosclerosis, increasing plaque vulnerability. Lifestyle choices, such as poor diet, physical inactivity, and excessive alcohol consumption, further exacerbate risk. Managing these factors through lifestyle modifications and medical therapies can significantly reduce the likelihood of ACS. Early intervention, such as quitting smoking and controlling blood pressure, is critical to mitigating cardiovascular risk and improving long-term outcomes.
2.2 Non-Modifiable Risk Factors
Non-modifiable risk factors for acute coronary syndrome (ACS) include age, gender, and genetic predisposition. Men typically have a higher risk than women before menopause, and the likelihood increases with advancing age. Family history of cardiovascular disease also plays a significant role. While these factors cannot be altered, understanding their impact allows for tailored risk assessment and monitoring. Recognizing these non-modifiable factors is crucial for early identification and management of individuals at higher risk for ACS.
2.3 The Role of Vulnerable Plaques
Vulnerable plaques play a critical role in the development of acute coronary syndrome (ACS). These plaques are characterized by a large lipid core, thin fibrous cap, and high macrophage density, making them prone to rupture. When a vulnerable plaque ruptures, it triggers an inflammatory response and thrombus formation, leading to sudden occlusion of the coronary artery. This process underlies the pathophysiology of ACS, including unstable angina and myocardial infarction. Identifying and stabilizing vulnerable plaques is a key target in both prevention and treatment strategies for ACS.

Clinical Presentation
Acute coronary syndrome (ACS) typically presents with chest pain or discomfort, often described as pressure or tightness radiating to the arm, neck, or jaw. Shortness of breath, sweating, nausea, or lightheadedness may accompany these symptoms, which can vary in intensity and duration. Prompt recognition of these signs is critical for early diagnosis and intervention.
3.1 Typical Symptoms of ACS
Chest pain or discomfort is the most common symptom of acute coronary syndrome (ACS), often described as a pressure, tightness, or heaviness in the chest. This pain may radiate to the arms, neck, jaw, or back. It is typically persistent, lasting more than a few minutes, and may worsen over time. Accompanying symptoms include shortness of breath, sweating, nausea, vomiting, lightheadedness, or fainting. Some patients may experience fatigue or indigestion-like discomfort. These symptoms often occur at rest or with minimal exertion and are critical for early diagnosis and intervention.
3.2 Atypical Symptoms and Silent Ischemia
Atypical symptoms of ACS may include epigastric discomfort, dyspnea, or fatigue without chest pain, particularly in women, older adults, or diabetic patients. Silent ischemia, where myocardial ischemia occurs without noticeable symptoms, is common in diabetics due to neuropathy. These presentations can delay diagnosis and treatment, emphasizing the need for a high index of suspicion in vulnerable populations. Early recognition is critical to prevent adverse outcomes, even when classic chest pain is absent.
3.3 Physical Examination Findings
Physical examination findings in ACS may include chest tenderness, diaphoresis, and signs of heart failure such as crackles or peripheral edema. Blood pressure may be elevated or hypotension present, indicating cardiogenic shock. A fourth heart sound (S4) is common due to decreased ventricular compliance. However, some patients may have no overt physical signs, particularly in the early stages. These findings, combined with clinical history, guide further diagnostic steps and management, ensuring timely intervention for optimal patient outcomes.

Diagnosis and Assessment
The diagnosis of acute coronary syndrome involves a combination of clinical evaluation, electrocardiography, biomarker detection, and imaging. Key steps include assessing symptoms, performing an ECG to identify ischemic changes, measuring troponin levels for myocardial injury, and using imaging techniques like echocardiography to evaluate cardiac function. Risk stratification tools, such as the GRACE score, help predict outcomes and guide management. Timely and accurate diagnosis is critical for initiating appropriate treatment and improving patient prognosis.
4.1 ECG Findings in ACS
The electrocardiogram (ECG) is a cornerstone in diagnosing acute coronary syndrome (ACS). Key findings include ST-segment elevation in STEMI, ST-segment depression, or T-wave inversion in NSTE-ACS. Q-waves may indicate prior myocardial infarction. The presence of ST-segment elevations is critical for distinguishing STEMI from other forms of ACS. ECG changes should be interpreted promptly, as they guide immediate management, including reperfusion therapy. Serial ECGs are recommended to monitor ischemia resolution and detect potential complications like arrhythmias. Timely ECG acquisition is vital for improving outcomes in ACS patients.
4.2 Biomarkers of Myocardial Injury
Biomarkers are essential for diagnosing myocardial injury in acute coronary syndrome (ACS). Elevated troponin levels (TnT or TnI) are highly sensitive and specific for myocardial infarction, making them a cornerstone in ACS diagnosis; Creatine kinase-MB (CK-MB) is another biomarker, though less specific than troponin. Myoglobin levels rise early after injury but lack specificity. B-type natriuretic peptide (BNP) and NT-proBNP are associated with heart failure and may indicate stress in ACS. These biomarkers help confirm myocardial damage and guide treatment decisions, with troponin remaining the most reliable indicator of infarction.
4.3 Imaging Techniques in ACS
Imaging techniques play a crucial role in diagnosing and managing acute coronary syndrome (ACS). Echocardiography is commonly used to assess left ventricular function and identify wall motion abnormalities, which may indicate ischemia. Coronary angiography remains the gold standard for visualizing coronary artery anatomy and identifying obstructive lesions. Other modalities like cardiac MRI and CT angiography provide detailed images of cardiac structure and coronary arteries, aiding in risk stratification and treatment planning. These tools complement clinical and biochemical assessments, ensuring accurate diagnosis and tailored interventions.
4.4 Risk Stratification Tools
Risk stratification tools are essential for identifying patients with acute coronary syndrome (ACS) who are at higher risk of adverse outcomes. The GRACE Risk Score and TIMI Risk Score are widely used to predict mortality and recurrence of ischemic events. These tools incorporate clinical variables such as age, troponin levels, ECG findings, and renal function. Accurate risk stratification guides management decisions, including the need for invasive strategies or medical therapy. Early identification of high-risk patients ensures timely interventions, improving outcomes and reducing long-term complications.

Management Strategies
Management of acute coronary syndrome involves immediate interventions, antiplatelet therapy, anticoagulants, and reperfusion strategies like PCI or fibrinolysis to restore blood flow and reduce ischemic damage.
5.1 Immediate Interventions
Immediate interventions for acute coronary syndrome focus on stabilizing the patient and restoring blood flow. Oxygen therapy is administered to increase oxygen delivery to the ischemic myocardium; Sublingual nitroglycerin is commonly used to relieve chest pain by dilating coronary arteries. Aspirin is promptly given to inhibit platelet aggregation, followed by P2Y12 inhibitors for additional antiplatelet therapy. Heparin or other anticoagulants may be administered to prevent further thrombus formation. Rapid ECG monitoring is critical to identify ST-segment elevations or depressions, guiding urgent reperfusion strategies such as PCI or fibrinolysis.
5.2 Medical Therapy in ACS
Medical therapy for acute coronary syndrome (ACS) aims to reduce ischemia, prevent further thrombosis, and improve survival. Aspirin is administered immediately to inhibit platelet aggregation. P2Y12 inhibitors, such as clopidogrel or ticagrelor, are added for dual antiplatelet therapy. Heparin or low-molecular-weight heparin is often used for anticoagulation. Beta-blockers reduce myocardial oxygen demand by lowering heart rate and blood pressure. High-dose statins are initiated to stabilize plaques and reduce inflammation. ACE inhibitors or ARBs may be prescribed for patients with hypertension or heart failure.
5.3 Invasive vs. Conservative Strategies
In managing acute coronary syndrome (ACS), the choice between invasive and conservative strategies depends on patient risk and clinical presentation. Invasive strategies, such as coronary angiography followed by percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG), are recommended for high-risk patients, including those with ongoing ischemia or elevated cardiac biomarkers. Conservative strategies, focusing on medical therapy and lifestyle modifications, are typically reserved for low-risk patients with stable symptoms. Guidelines emphasize individualized decision-making, balancing benefits of early intervention against procedural risks.
5.4 Secondary Prevention Measures
Secondary prevention in acute coronary syndrome (ACS) aims to reduce long-term cardiovascular risks and improve patient outcomes. Key measures include lifestyle modifications such as smoking cessation, a heart-healthy diet, regular exercise, and weight management. Medications like statins, beta-blockers, ACE inhibitors, and antiplatelet agents are cornerstone therapies to lower cholesterol, blood pressure, and clotting risk. Cardiac rehabilitation programs are also recommended to enhance recovery and reduce future event rates. These strategies are tailored to individual risk profiles and comorbidities, ensuring comprehensive and sustained care post-ACS.

Complications and Prognosis
ACS can lead to complications like arrhythmias, heart failure, or sudden cardiac death. Prognosis varies based on severity, treatment response, and underlying health conditions, impacting long-term outcomes significantly.
6.1 Short-Term Complications of ACS
Acute coronary syndrome (ACS) can lead to serious short-term complications, including arrhythmias, such as ventricular fibrillation, and heart failure due to reduced ejection fraction. Cardiogenic shock, a life-threatening condition, may occur if the heart cannot pump enough blood. Additionally, mechanical complications like mitral regurgitation or ventricular septal defects can arise from myocardial rupture. Early recognition and treatment are critical to mitigating these risks and improving patient outcomes.
6.2 Long-Term Prognosis and Outcomes
The long-term prognosis for acute coronary syndrome (ACS) varies depending on the severity of initial cardiac damage and comorbidities. Patients with significant myocardial infarction may develop heart failure, while others experience recurrent ischemia. Guideline-directed therapies, including beta-blockers and statins, improve survival and reduce recurrence. Cardiac rehabilitation programs further enhance functional recovery and quality of life. Long-term adherence to lifestyle modifications, such as diet and exercise, is crucial for minimizing the risk of further events and improving overall outcomes.
6.3 Impact of Socioeconomic Factors
Socioeconomic factors significantly influence the incidence, management, and outcomes of acute coronary syndrome (ACS). Disparities in income, education, and access to healthcare contribute to delayed diagnosis and treatment, particularly in underserved populations. Lower socioeconomic status is associated with reduced access to guideline-directed therapies, medications, and rehabilitation programs. Geographical variations further exacerbate these inequalities, with higher rates of ACS-related complications observed in regions with limited healthcare resources. Addressing these disparities is essential to improving outcomes and reducing the societal burden of ACS.

Prevention and Rehabilitation
Preventing ACS involves lifestyle changes, such as diet modification, smoking cessation, and regular exercise. Rehabilitation programs focus on improving heart health, reducing risk factors, and enhancing recovery.
7.1 Lifestyle Modifications
Lifestyle changes are crucial in preventing ACS and improving outcomes. A heart-healthy diet, such as the Mediterranean diet, reduces saturated fats and increases fiber, fruits, and vegetables. Regular physical activity, like moderate exercise, enhances cardiovascular health. Smoking cessation significantly lowers cardiovascular risk. Stress management through techniques like yoga or meditation also plays a role. These modifications aim to reduce modifiable risk factors, improve overall well-being, and decrease the likelihood of future cardiac events. Patient education and monitoring are essential for long-term adherence to these changes.
7.2 Cardiac Rehabilitation Programs
Cardiac rehabilitation programs are structured interventions designed to help patients recover from ACS and reduce future cardiovascular risks. These programs typically include supervised exercise, education on heart-healthy lifestyles, and psychological support. They aim to improve physical function, reduce symptoms, and enhance overall well-being. Participation in cardiac rehab has been shown to improve prognosis, reduce hospital readmissions, and increase quality of life. These programs are usually tailored to individual needs and may involve monitoring of progress by a multidisciplinary team of healthcare professionals.
7;3 Public Health Initiatives
Public health initiatives play a crucial role in reducing the burden of acute coronary syndrome (ACS) by promoting preventive measures and early intervention. These initiatives include educational campaigns to raise awareness about ACS symptoms, risk factors, and the importance of timely medical care. Community-based programs often focus on lifestyle modifications, such as healthy diet, regular physical activity, and smoking cessation. Additionally, partnerships with healthcare organizations and policymakers help implement guidelines and improve access to cardiovascular care, ultimately aiming to reduce ACS incidence and improve population health outcomes.
Recent Advances and Guidelines
Recent advances in ACS management include the emergence of novel antiplatelet therapies and updated 2023 ESC guidelines emphasizing early intervention and personalized treatment strategies.
8.1 Emerging Therapies in ACS
Emerging therapies in acute coronary syndrome (ACS) focus on novel antiplatelet agents and anticoagulants to reduce ischemic events. Recent advancements include the development of newer P2Y12 inhibitors and factor XIa inhibitors, which offer improved efficacy with lower bleeding risks. Additionally, therapies targeting inflammation, such as interleukin-1β inhibitors, are being explored to stabilize vulnerable plaques. The use of intravenous nitroglycerin and sodium nitroprusside for rapid vasodilation is also gaining traction. These innovations, alongside advancements in percutaneous coronary intervention (PCI) techniques, aim to enhance outcomes and reduce complications in ACS patients.
8.2 2023 ESC Guidelines Overview
The 2023 ESC Guidelines for acute coronary syndrome (ACS) emphasize evidence-based management strategies. Key recommendations include the use of dual antiplatelet therapy (DAPT) for up to 12 months in high-risk patients and the preference for P2Y12 inhibitors over clopidogrel. The guidelines also stress the importance of assessing ischemic and bleeding risks to tailor treatment. High-intensity statins are recommended for all ACS patients, and invasive strategies are prioritized for high-risk cases. These updates aim to optimize outcomes, reduce complications, and standardize care across clinical settings.

Special Populations
Acute coronary syndrome (ACS) presents differently in women, younger individuals, and those with comorbidities, requiring tailored management strategies to address unique risk factors and improve outcomes.
9.1 Gender Differences in ACS
Gender differences in acute coronary syndrome (ACS) are significant, with women often presenting with atypical symptoms such as shortness of breath or fatigue rather than chest pain. Women also tend to experience worse outcomes due to delays in diagnosis and treatment. Pathophysiological differences, including smaller coronary artery size and higher prevalence of plaque erosion, contribute to these disparities. Additionally, socioeconomic factors and comorbidities like diabetes disproportionately affect women, necessitating tailored management strategies to improve outcomes in female ACS patients.
9.2 ACS in Younger Patients
Acute coronary syndrome (ACS) in younger patients is relatively rare but remains a significant concern. Studies show that younger individuals, particularly those under 40, often present with fewer traditional risk factors like hypertension or diabetes. Instead, lifestyle factors such as smoking, substance abuse (e.g., cocaine use), and premature atherosclerosis play a larger role. Genetic predispositions and familial hypercholesterolemia are also more common in this group. Despite this, younger patients generally have better short-term outcomes compared to older cohorts, though long-term cardiovascular risks remain elevated.
9.3 Management in Patients with Comorbidities
Management of ACS in patients with comorbidities requires a tailored approach to address both the acute condition and underlying health issues. Comorbidities such as diabetes, hypertension, and chronic kidney disease can complicate treatment and worsen outcomes. Optimal care involves medications like beta-blockers, statins, and ACE inhibitors, with careful consideration of dosage adjustments. Additionally, controlling blood glucose levels and managing hypertension is crucial. A multidisciplinary team approach ensures comprehensive care, improving both short- and long-term outcomes for these high-risk patients while minimizing complications.
Acute coronary syndrome is a critical condition requiring prompt intervention. Early diagnosis, evidence-based treatments, and lifestyle modifications are essential for improving outcomes and reducing recurrence risk.
10.1 Summary of Key Points
Acute coronary syndrome (ACS) encompasses unstable angina, non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI), caused by reduced coronary blood flow. Early diagnosis via ECG, biomarkers, and imaging is critical for timely intervention. Treatment strategies include revascularization, medical therapy, and lifestyle modifications. Secondary prevention measures, such as antiplatelet therapy and statins, reduce recurrence risk. Addressing modifiable risk factors and socioeconomic disparities is essential for improving outcomes. Public health initiatives and cardiac rehabilitation further enhance long-term prognosis and quality of life.
10.2 Future Directions in ACS Management
Future directions in ACS management focus on personalized medicine, leveraging genomics and precision therapies. Emerging therapies, such as anti-inflammatory drugs and cell-based therapies, aim to reduce myocardial damage. Enhanced imaging and biomarkers will improve early detection and risk stratification. Wearable technology and telemedicine will enable remote monitoring, reducing complications. Addressing socioeconomic disparities and improving global access to care are key priorities. Integration of the 2023 ESC Guidelines into clinical practice will further optimize outcomes, ensuring evidence-based care is universally accessible and effective.




